Gastrectomy
Surgery - stomach removal; Gastrectomy - total; Gastrectomy - partial; Stomach cancer - gastrectomy
Gastrectomy is surgery to remove part or all of the stomach.
- If only part of the stomach is removed, it is called partial gastrectomy
- If the whole stomach is removed, it is called total gastrectomy
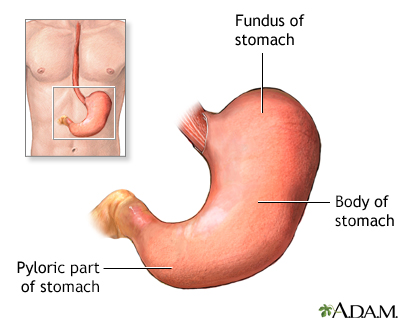
The stomach is divided into three parts, the fundus, the body and the pyloric part.
Description
The surgery is done while you are under general anesthesia (asleep and pain free). The surgeon makes a cut in the abdomen and removes all or part of the stomach, depending on the reason for the procedure.
Depending on what part of the stomach was removed, the intestine may need to be reconnected to the remaining stomach (partial gastrectomy) or to the esophagus (total gastrectomy).
Some surgeons can also do this surgery using a laparoscope. A laparoscope has a tiny camera that is inserted into your belly through a small cut. Video from the camera will appear on a monitor in the operating room. The surgeon views the monitor to do the surgery. When done this way, the surgery, which is called laparoscopy, is done with a few small surgical cuts. The advantages of this surgery are a faster recovery, less pain, and only a few small cuts.
Why the Procedure Is Performed
This surgery is used to treat stomach problems such as:
- Bleeding
- Inflammation
- Cancer
- Polyps (growth on the lining of the stomach)
Risks
Risks for anesthesia and surgery in general include:
- Reactions to medicines or breathing problems
- Bleeding, blood clots, heart problems. or infection
Risks for this surgery include:
- Leaking from the connection to the intestine which can cause infection or abscess
- Narrowing of the connection to the intestine, causing blockage
- Nausea or vomiting
- Dumping syndrome, (when food moves too rapidly from the stomach to the duodenum)
- Persistent diarrhea
Before the Procedure
If you are a smoker, you should stop smoking several weeks before surgery and not start smoking again after surgery. Smoking slows recovery and increases the risk of problems. Tell your surgeon or health care provider if you need help quitting.
Tell your surgeon or nurse if:
- You are or could be pregnant
- You are taking any medicines, including medicines, supplements, or herbs you bought without a prescription
During the week before your surgery:
- You may be asked to temporarily stop taking medicines that keep your blood from clotting. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
You may stay in hospital for 6 to10 days.
After surgery, there may be a tube in your nose which will help keep your stomach empty. It is removed as soon as your bowels are working well.
Most people have pain from the surgery. You may receive a single medicine or a combination of medicines to control your pain. Tell your surgeon when you are having pain and if the medicines you are receiving control your pain.
How well you do after surgery depends on the reason for the surgery and your condition.
Ask your surgeon if there are any activities you shouldn't do after you go home. It may take several weeks for you to recover fully. While you are taking narcotic pain medicines, you should not drive.
References
Antiporda M, Reavis KM. Gastrectomy. In: Delaney CP, ed. Netter's Surgical Anatomy and Approaches. 2nd ed. Philadelphia, PA: Elsevier; 2021:chap 8.
Mahvi DA, Mahvi DM. Stomach. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 49.
Version Info
Last reviewed on: 9/30/2024
Reviewed by: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
