Pityriasis rubra pilaris
PRP; Pityriasis pilaris; Lichen ruber acuminatus; Devergie disease
Pityriasis rubra pilaris (PRP) is a rare skin disorder that causes inflammation and scaling (exfoliation) of the skin.

This person has pityriasis rubra pilarisis on the chest, an uncommon skin condition characterized by salmon-colored patches with scaling (palmoplantar keratoderma). A characteristic sign of pityriasis rubra pilaris is plugging of the hair follicles with keratin. This picture illustrates areas of uninvolved skin (islands of sparing) surrounded by areas of redness (erythroderma).

This is a picture of pityriasis rubra pilaris on the feet. It is an uncommon skin condition characterized by thick scales and salmon-colored patches.

This is a picture of pityriasis rubra pilaris on the palms. This is an uncommon skin condition characterized by salmon-colored patches with scaling (palmoplantar keratoderma).
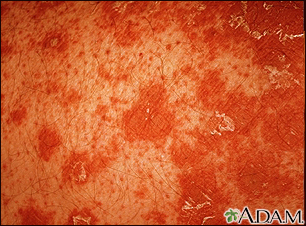
Pityriasis rubra pilaris is an uncommon skin condition. It is characterized by salmon-colored patches with scaling, clear areas of normal skin, and thick palms and soles. Hair follicles with keratin plugging is a characteristic sign. Typically the follicle is surrounded with a characteristic orange-red color.

This picture shows pitted, flesh colored pits (keratolysis) or depressions on the soles of the feet, associated with a bad odor (mal-odor). This is thought to be caused by overgrowth of diptheroids and micrococcus.
Causes
There are several subtypes of PRP. The cause is unknown, although genetic factors and an abnormal immune response may be involved. One subtype is associated with HIV/AIDS.
Symptoms
PRP is a chronic skin condition in which orange or salmon-colored scaly patches with thick skin develop on the hands and feet.
The scaly areas may cover much of the body. Small islands of normal skin (called islands of sparing) are seen within the areas of the scaly skin. The scaly areas may be itchy. There may be changes in the nails.
PRP can be severe. Although it's not life threatening, PRP can greatly reduce quality of life and limit activities of daily living.
Exams and Tests
Your health care provider will examine your skin. The diagnosis is usually made by the presence of the unique skin lesions. (A lesion is an abnormal area on the skin). Your provider may take samples (biopsies) of the affected skin to confirm the diagnosis and rule out conditions that may look like PRP.
Treatment
Topical creams containing urea, lactic acid, retinoids, and steroids may help. More commonly, treatment includes pills taken by mouth such as isotretinoin, acitretin, or methotrexate. Exposure to ultraviolet light (light therapy) may also help. Medicines that affect the body's immune system are currently being studied and may be effective for PRP.
Support Groups
More information and support for people with PRP disorder and their families can be found at:
- Genetic and Rare Diseases Information Center.
rarediseases.info.nih.gov/diseases/7401/pityriasis-rubra-pilaris - National Organization for Rare Disorders --
rarediseases.org/rare-diseases/pityriasis-rubra-pilaris/
When to Contact a Medical Professional
Contact your provider if you develop symptoms of PRP. Also contact your provider if you have the disorder and symptoms worsen.
References
James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM. Pityriasis rosea, pityriasis rubra pilaris, and other papulosquamous and hyperkeratotic diseases. In: James WD, Elston DM, Treat JR, Rosenbach MA, Neuhaus IM, eds. Andrews' Diseases of the Skin: Clinical Dermatology. 13th ed. Philadelphia, PA: Elsevier; 2020:chap 11.
Patterson JW. Disorders of pigmentation. In: Patterson JW, ed. Weedon's Skin Pathology. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 11.
Version Info
Last reviewed on: 5/31/2023
Reviewed by: Ramin Fathi, MD, FAAD, Director, Phoenix Surgical Dermatology Group, Phoenix, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 01/14/2025.
